Introduction
CVA is a disruption of cerebral circulation that leads to motor and sensory deficit. This is the most common cerebrovascular conditions. It has got several synonyms e.g. brain attack or apoplexy.
Stroke is an emergency that requires immediate attention so as to prevent neurological deficit and permanent disability.
 |
| Photo by Mayo Clinic |
Types of CVAs
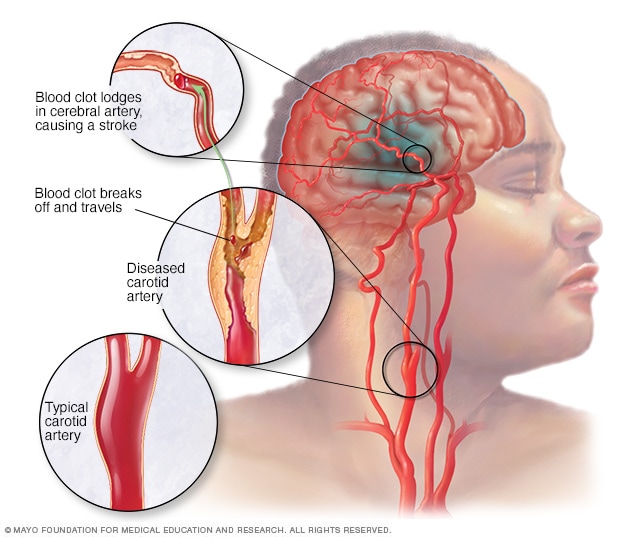
- Ischemic (occlusive); this occur as a result of occlusion of blood vessel by embolus (embolic stroke) or thrombus (thrombotic stroke).
- Haemorrhagic stroke; this results from interruption of blood vessels integrated with bleeding into the brain tissue or surrounding spaces.
Incidence
Stroke is the leading cause of death and disability in the world. About 700,000 people suffer stroke each year and in every 45 seconds, someone suffer from stroke and dies of stroke every 3 minutes. It is common in older people over 65 years of age and occurs more frequently in men than in women. (American heart association, 2005).
Risk Factors
- People living with hypertension has a four to six time greater risk for stroke than those living without.
- Heart diseases e.g. atrial fibrillation, mitral valve stenosis, patent foramen ovale and cardiac surgery.
- Diabetes mellitus may leads to vascular changes in both systemic and cerebral circulation increasing the risk of hypertension.
- Blood cholesterol levels i.e. risks of atherosclerosis.
- Smoking doubles a person’s risk for ischemic/hemorrhagic stroke and common in young adults.
- Sickle cell disease causes increase in blood viscosity and erythrocyte clumps and occlude the small vessels.
- Substance abuse; injection of unpurified substances increase the risk of stroke and abuse of certain drugs decrease blood flow and increase risk of intracranial haemorrhage.
- African descent; high prevalence of hypertension
- Family history of stroke
- Obesity
- Sedentary lifestyle especially where there is a lack of exercise.
- Previous transient ischemic attack (TIA).
Aetiology
- Cerebral arteriosclerosis
- Syphilis; septic embolism
- Trauma
- Hypertension
- Haemorrhage
- Occlusion of artery by embolus or thrombus
- Ruptured aneurysm
Pathophysiology
When the cerebral arteries become blocked as result of embolus or thrombus, auto-regulatory mechanism helps maintain cerebral circulation until collateral circulation develops to deliver blood to the affected area.
Impaired cerebral blood flow for more than 4minutes causes oxygen deprivation which leads to infarction of brain tissue. Neurons served by the occluded vessel die from lack of oxygen and nutrient resulting in cerebral infarction. Accumulation of calcium, sodium and water in the injured cells leads to release of excitatory neurotransmitters causing further cell injury and swelling.
When hemorrhage is the cause, impaired cerebral perfusion causes infarction and the blood itself acts as a space-occupying lesion mass. The brain’s regulatory mechanism attempts to maintain equilibrium by increasing blood pressure to maintain cerebral perfusion pressure. The increased Intracranial Pressure forces Cerebrospinal Fluid out impairing absorption and circulation which leads to damage of brain cells.
Clinical Manifestation
The clinical features of CVA is highly dependent upon size and site of lesion.
- Motor loss or changes
- Hemiplegia; paralysis on one side of the body.
- Hemiparesis; motor weakness on one side of the body.
- Communication loss
- Receptive aphasia; inability to understand spoken word.
- Expressive aphasia; inability to speak.
- Vision loss.
- Sensory loss
- Paresthesia and Bladder impairment.
- Impaired mental activity.
- Altered LOC may vary from lethargy, to mental confusion to deep coma.
- Blood pressure elevated due to increased Intracranial Pressure.
- Sudden, severe headache with nausea and vomiting seizures
- Cognitive changes affecting the brain includes; right cerebral hemisphere damage affects Vision.
- Spatial (space) awareness.
- Proprioception (information concerning movement and position of the body) thus there are changes in time, place, personality (e.g. impulsivity and poor judgment).
- Left cerebral hemisphere damage gives rise to Aphasia.
- Alexia (word blindness) and Agraphia (absence of the power of expressing though in writing).
- Hypotonia and flaccidity; the patient is unable to overcome the forces of gravity so that the extremities fall to the side. The extremities feel heavy and the muscle tone is insufficient for balance, equilibrium or protective mechanism.
- Hypertonic (spastic paralysis). This causes fixed positions/contractures of involved extremities. ROM is also restricted and subluxation can easily occur from spasticity or flaccidity.
- Sensory perceptual deficits; this involves responses to painful stimuli or touch.
- Agnosia; inability to recognize one or more subject that were previously known, may be visual tactile or auditory.
- Apraxia; patient is not able to write, comprehend reading material or carry out a purposeful activity.
- Neglect syndrome where patient is not aware of paralyzed side (common in right hemisphere).
- Pupillary abnormalities e.g. ptosis (drooping of eyes), visual defects, pallor/petechiae due to infarction or ischemia of carotid artery.
- Hemianopsia; blindness in half of the visual (field), Homonymous hemianopsia; when this occurs in same sides of both eyes.
Cranial nerve (CN) intactness impairment includes;
- CN5 - chewing
- CN9 and 10 – swallowing
- The difficulty in chewing and swallowing can have aspiration pneumonia or constipation from insufficient fluid intake.
- CN7 - facial paresis
- CN9 - absence of gag reflex
- CN12 - impaired tongue movement
Diagnosis investigation
- Blood; prothrombin time and partial prothrombin time, to set base line data.
- Cerebrospinal Fluid (CSF) analysis
- CT-scan to determine intracranial bleeding, infarcts or shifts of the midline structures; brain to determine decreased perfusion.
- Electroencephalogram (EEG) - to show focal slowing in the lesion area.
/eeg-601235088-5a524fdef1300a0037eeebe5.jpg)
Photo by Verywell Health - Magnetic resonance imaging (MRI) - determine intracranial bleeding, infarcts or shift or the midline structures; to determine decreased perfusion, presence of oedema and tissue necrosis.
- Angiography cerebral digital sub traction/magnetic resonance to determine status of cerebral vessels.
- Radiology - skull x-ray to help detect presence of abnormal calcification of blood vessels or pineal shift, both indicates the presence of cerebral haemorrhage.
Management
- Medical and nursing management in the acute phase of CVA
The objective of care during the acute phase includes;
- Keep the patient alive.
- Minimize cerebral damage to providing adequately oxygenated blood to the brain.
- Support airway, breathing and circulation (ABC).
- Provide quiet environment to ensure rest.
- Assess neurological status - level of consciousness (LOC)
- Pupil size and reaction of light
- Patients response to command
- Movement and strength,
- Patients vital signs
- Continually reorient patient to person, place and time.
- Maintain proper positioning/body alignment
- Prevent complications of bed rest
- Nurse patient in semi-fowlers position
- Apply foot board, sand bags, trochanter rolls and splints as necessary
- Keep head of bed elevated 30degrees to reduce HCP
- Turn patient every 2 hours to maintain skin integrity
- Ensure adequate fluid and electrolyte balance — IVF are maintained until condition stabilizes then nasogastric feedings or oral feeding depending on patient’s abilities.
- Administer medications as ordered. Anti-hypertensive, antibiotics, anticonvulsants, anticoagulants. Note that sedatives and tranquilizer are not given because they depress respiratory center and obscure neurological observation.
- Maintain adequate elimination – urethral catheter may be passed during acute phase and bladder retraining is begun during rehabilitation phase.
- Provide stool softeners to prevent constipation.
- Monitor for seizures/protect patient from injure.
- Include patient’s family and significant others in plan of care.
- Rehabilitation of the patient after Cerebrovascular Accident
Under rehabilitation to stroke patients, multidisciplinary team is most frequently utilized.
- Development of behavior patterns which is likely to prevent the recurrence of Symptoms:
- Taking prescribed medication
- Stopping smoking
- Reducing day to day stress
- Modifying diet
- Physiotherapy; passive and active ROM and isometric exercises.
- Education – to client; on causes and management, specific teaching, encouragement and support. Counseling and support to family is an integral part of rehabilitation process.
- Speech therapy may be necessary.
Surgical intervention
- Carotid endarterectomy (surgical removal of part of the inner lining of an artery, together with any obstructive deposits).
- Craniotomy for evacuation of clot.
- Craniotomy for superior temporal artery.
Read Also









0 Comments