Diabetes is a chronic and potentially disabling disease characterized by elevated blood sugar levels. Diabetes Mellitus (DM) causes alternations in metabolism of carbohydrates, proteins and fats.
Carbohydrates are the body's preferred source of energy. Once digested, carbohydrates are converted into glucose and provide necessary nutrients for the body Through careful release of insulin, the body is able to control how and when fats, protein and carbohydrates are metabolized.
Insulin is released continuously by the pancreas according to the needs of the body.
CLASSIFICATION OF DIABETES MELLITUS
TYPE 1 DIABETES
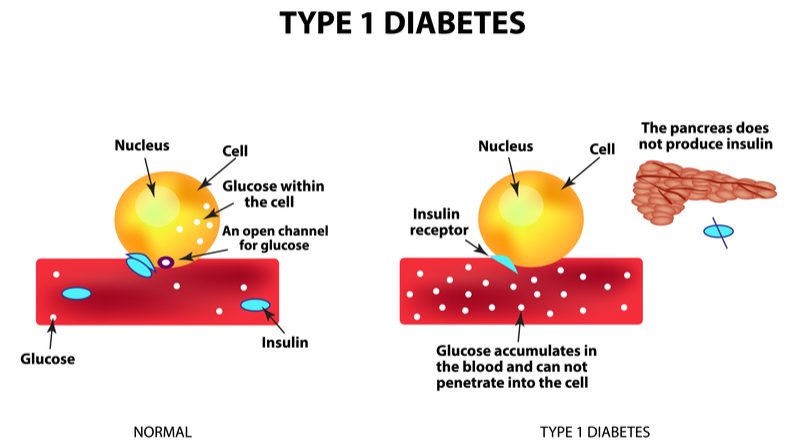
INSULIN DEPENDENT DIABETES MELLITUS (IDDM); In type 1, genetics or viruses or autoimmune response alone or in combination are involved. About 5-10% of people with diabetes have this type. Most people with this type are diagnosed before the age 30. There is inadequate supply of insulin. In this type, patients need exogenous type of insulin.
WHAT HAPPENS? Type 1 diabetes results from the destruction of the beta cells in the islet of Langerhans in the pancreas. This destruction usually results from immunological defects that produces antibodies against the beta cells. These antibodies may be present for months or years before clinical symptoms of diabetes develop. So lets just say, your body's soldiers fight against your pancreas in this type.
 |
| Photo by nurseslabs.com |
SIGNS AND SYMPTOMS
When diagnosed, individuals have these four cardinal manifestations;
1. Weight loss and muscular wasting due to breakdown of protein and lipids (catabolism).
2. Polyuria; frequent urination because glucose attracts water and an osmotic dieresis occur. This polyuria leads to a loss of water and electrolyte, particularly Na, Cl, K and phosphate.
3. Polydypsia; The loss of water and sodium results in thirst and increase in fluid intake.
4. Polyphagia; Extreme hunger and increased food intake are triggered as the cells become starved of their fuel.
DM patients are known to easily get tied.
In addition
1. It usually begins in childhood but may occur at any age.
2. Measurable circulating insulin may still be present early in the course of the disease but soon disappears
3. As insulin production decreases, hyperglycemia develop as a result of the body's inability to use glucose.
4. It the concentration of glucose in the blood is sufficiently high, kidneys may not reabsorb all the filtered glucose; the glucose then appears in urine (Glucosuria). Fluid lose through the kidneys results as the kidney works to excrete the increased load of glucose, producing loss of water, sodium, magnesium, calcium, potassium, chloride and phosphate.
KETOACIDOSIS
When there is deficiency in insulin, muscles cannot utilize glucose. Free fatty acids are then mobilized from the adipose tissue cells and broken down by the liver into ketone bodies for energy. In other words, there is a severe lack of insulin. For this reason the blood glucose, although very high, cannot be utilized for energy production. Fat is broken down instead, producing toxic, chemicals called ketone. Ketoacidosis is therefore characterized by excessive ketone bodies in the blood. Patients with ketoacidosis exhibit hyperventilation and loss of Na, KCl and water from the body. This could cause severe dehydration and electrolyte imbalance.
Often the diagnosis of DM is first made when the patient is brought to the hospital in coma state due to ketoacidosis. Diabetic ketoacidosis is the commonest cause of death among diabetics in Ghana.
Cause
1. Previously undiagnosed diabetes
2. Interruption of insulin therapy (usually for financial reasons or for alternative treatment)
3. Stress of undercurrent illness (e.g infection, myocardial infraction, stroke etc)
Signs and symptoms
1. Passing excess urine
2. Dehydration with dry skins, reduced skin turgor or sunken eyes
3. Drinking excess amount of water
4. Relatives may report alteration in sensoruim or collapse
5. Deep and fast breathing etc.
Investigations
1. Blood glucose is usually greater that 18mmol/L
2. Urine glucose is usually more than 3+
3. Urine ketone usually higher than 2+
4. Blood urea, potassium and electrolytes are usually low, however if in renal failure urea and potassium are high.
TYPE 2 DIABETES
NON-INSULIN DEPENDENT DIABETES MELLITUS (NIDDM)
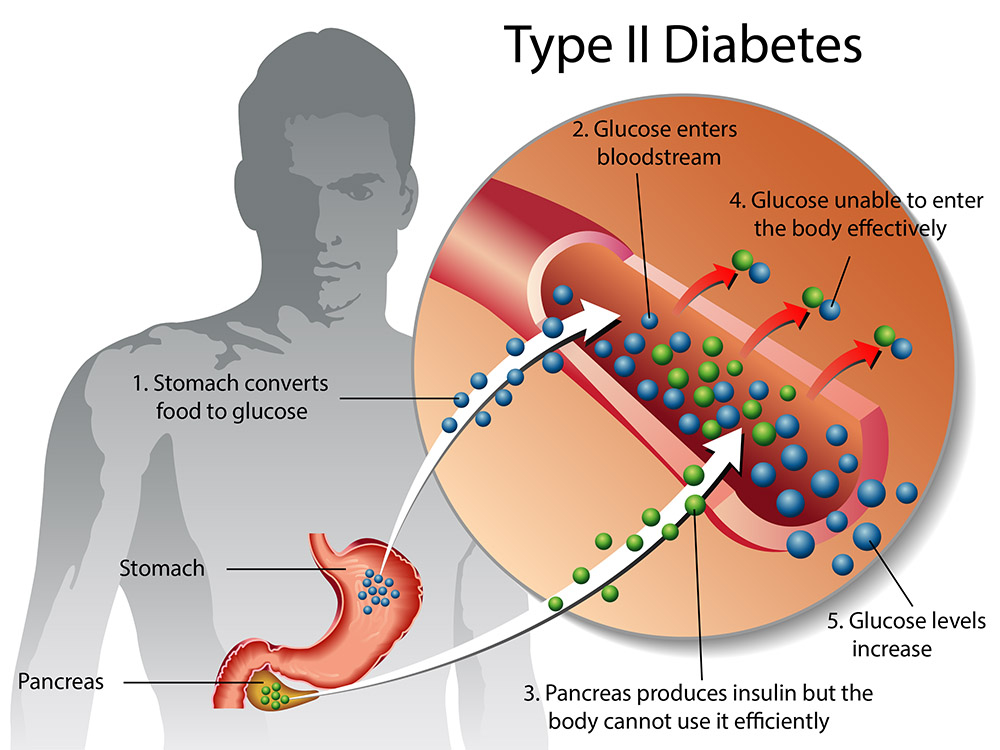
In type 2 DM, genetics and obesity play a more significant role. The exact role that heredity and obesity play is not completely understood, though they contribute. There is apparently no relationship between viruses and etiology of NIDDM.
It results from decrease in the amount of insulin produced or an insensitivity of cell to insulin. About 90-95% of the people with diabetes have type 2. Individuals have onset after age 40 years. Classic symptoms are not present when first diagnosed. In some non-insulin dependent diabetes patients, insulin secretion is increased resulting in higher circulating insulin levels but it is not utilized because of an inadequate number of insulin receptors present in cells.
This mechanism has been observed in obese non-insulin dependent patients. With weight loss, the number of insulin receptors on the cell increase, thereby allowing glucose to enter the cell. This may result in return of normal glucose utilization.
 |
| Photo by media.healthdirect.org.au |
In general
1. These patients may never require insulin and are usually managed adequately with diet alone
2. The majority i.e. about 80% of NIDDM patients are overweight when the condition is first diagnosed.
3. Symptoms my be so minor that the disease is undetected for many years.
4. Diagnosis may be suspected as a result of routine urinalysis.
5. Usually, the disease is discovered when the patient seeks health care treatment of complications such as deteriorating vision, pain in legs or impotence.
6. Often, blood sugar (glucose) tests are normal, with hyperglycemia been seen only in postprandial (following a meal).
GESTATIONAL DIABETES MELLITUS (GDM)
GDM applies only to women in whom glucose intolerance develops or discovered during pregnancy. After pregnancy, diagnostic classification may be changed to IDDM or NIDDM. Women who had the disease before pregnancy are not inclusive. Women with GDM have an increase future risk for progressive to NIDDM or rarely IDDM.
Effects of Pregnancy on Diabetes
Pregnancy is diabetogenic due to increased production of insulin antagonists such as human placental lactogen, placental insulinase, cortisol, estrogen and progesterone. Insulin requirements increase during pregnancy while it reduces postpartum.
DIAGNOSIS OF DIABETES MELLITUS
1. Based on classic symptoms which are polyuria, polydypsia, polyphagia, rapid weight loss.
2. The presence of abnormally high blood glucose levels is the criterion on which the diagnosis of diabetes should be based. An elevation in blood glucose for more than one occasion.
3. Elevated fasting blood glucose on more than one occasion.
4. Glucose Tolerance Test; Oral Glucose Tolerance Test and Intravenous Glucose Tolerance Test.
5. Urine test should not be used because both false-negative (renal threshold levels are higher than normal so no glucose is found in the urine despite elevated blood glucose value)and false-positive result (glucose appears in the urine despite normal glucose values in the elderly) occur.
MANAGEMENT OF DIABETES MELLITUS
Management of Diabetes Mellitus should be worked around therapeutics, relief of symptoms and maintaining Fasting Blood Sugar (FBS) within normal limits, preventing acute DM complications e.g. hypoglycemia, ketoacidosis etc and preventing chronic complication of diabetes such as blindness, amputation, kidney disease and nerve damage.
MEDICATION
a. Insulin
b. Biguanides such as Metformin hydrochloride with or soon after meals. Metformin decreases insulin resistance and increases insulin sensitization.
c. Sulphonylureas such as Tolbutamide, Gliclazide, Glibenclamide, Chlorpropamide etc. Sulphonylureas are best taken with meals.
{Drug Dosages withheld, consult your medical nursing tutor or a physician}.
NOTE: Two different Sulphonylureas should NEVER be used together. In older patients who usually have type 2 diabetes, diet alone should be tried first, when diet fails to achieve satisfactory control, non-obese patients are usually treated with Sulphonylureas drugs and obese patients with a Biguanide.
Avoid metformin and long-acting oral anti-diabetes drugs such as chlopronamide and Glibenclamide in individuals with poor kidney and liver functions. Oral anti-diabetic drugs should be avoided in type 1 patients and should not be used during pregnancy and breast-feeding, insulin is indicated instead.
Insulin is always indicated in patients who have been in ketoacidosis and in most young patients who usually have type 1 diabetes.
DIET (MEAL PLAN)
What ever meal a diabetic patient takes, be it breakfast, Lunch, afternoon snack, supper or bedtime, remember all diabetics require diet therapy. In general, patients must avoid 'free' or refined sugars, such as soft drinks and adding sugar to their beverages. Diet or soft drinks which contain a sweetener and not glucose may however be used. They shouldn't eat plenty at a time and should encourage enough fibre intakes.
EXERCISE (ACTIVITY)
Diet and exercise may be used to control blood glucose levels in individuals with type 2 DM but when the response to these measures is inadequate, oral agents are tried. Regular and simple exercise such as walking 1 hour daily is helpful in ensuring good glucose control. Advice on exercise however must give consideration to the patient's age and the presence of complications and other medical conditions.
In both type 1 and 2 DM, activity sensitizes insulin and enhance glucose uptake into skeletal muscles. The mechanism is unknown but exercise is an important part of medical management and should be observed with careful and thorough explanation before implementation. NOTE that the risk of exercise is hypoglycemia which is a diabetic emergency.
Benefits of Exercise
Improves insulin sensitivity
Lowers blood glucose
Assists with weight loss
Preserve with cardiovascular fitness
Improves sense of well-being.
MONITORING can be done with the [Sliding Scale]
NURSING MANAGEMENT OF DM
1. Physical Examination
2. Patient Education and psychological care; this should be on insulin self-administration, dispel of myths about DM, helping client to manage stress and psychological adjustment - if the patient is overwhelmed with emotions tell them it is okay to cry, adaptation of living with chronic disease.
3. Involve the family of the patient to provide social support, let them know that diabetes is a family challenge.
4. Promote adequate nutrition. Consider these diets;
a. Non-starchy vegetables such as broccoli, carrots, greens, peppers, and tomatoes
b. Fruits such as oranges, melon, berries, apples, bananas, and grapes
c. Grains such as wheat, rice, oats, cornmeal, barley, and quinoa examples bread, pasta, cereal, and tortillas
d. Protein such as lean meat, chicken or turkey without the skin, fish, eggs, nuts and peanuts, dried beans and certain peas, such as chickpeas and split peas, meat substitutes, such as tofu, Non-fat or low fat diary such as milk or lactose, yogurt, cheese.
5. Managing medications.
Read Also








0 Comments