Effects of Antepartum Haemorrhage
Effects on the Fetus
- Fetal mortality and morbidity are increased as a result of severe vaginal bleeding in pregnancy.
- Still birth and perinatal or neonatal death may occur.
- Premature placental separation and consequent hypoxia may result in birth of a child who is mentally and physically handicap,
Effects on the Mother
- If bleeding is severe, it may be accompanied by shock, disseminated intravascular coagulation and renal failure.
- The mother may die or be left with permanent ill-health.
Types of Antepartum Haemorrhage
Vaginal bleeding in late pregnancy is confined to placental separation due to placenta praevia or placental abruption.
PLACENTA PRAEVIA
The placenta is partially or wholly implanted in the lower uterine segment on either the anterior or posterior wall. The lower uterine segment grow and stretches progressively often within the 12th week of pregnancy. In late weeks, this may cause the placenta to separate and severe bleeding can occur.
Type 1 Placenta Praevia
- The majority of the placenta is in the upper uterine segment.
- Vaginal delivery is possible.
- Blood loss is usually mild.
- The mother and the fetus remains in good condition.
Type 2 Placenta Praevia
- The placenta is partially located in the lower uterine segment near the internal os (Marginal placenta praevia.
- Vaginal delivery is possible particularly if the placenta is implanted anteriorly.
- Blood loss is usually moderate.
- Fetal hypoxia is more likely to be present.
Type 3 Placenta Praevia
- The placenta is located centrally over the internal opening of the cervix.
- Bleeding is likely to be severe. Particularly, when the lower segment stretches and the cervix begins to efface and dilate in late pregnancy.
- Vaginal delivery is inappropriate.
Type 4 Placenta Praevia
- The placenta is located centrally over the internal cervical os and severe haemorrhage is very likely.
- Vaginal delivery should not be considered.
- Caesarean section is essential in order to save the life of the mother and fetus.
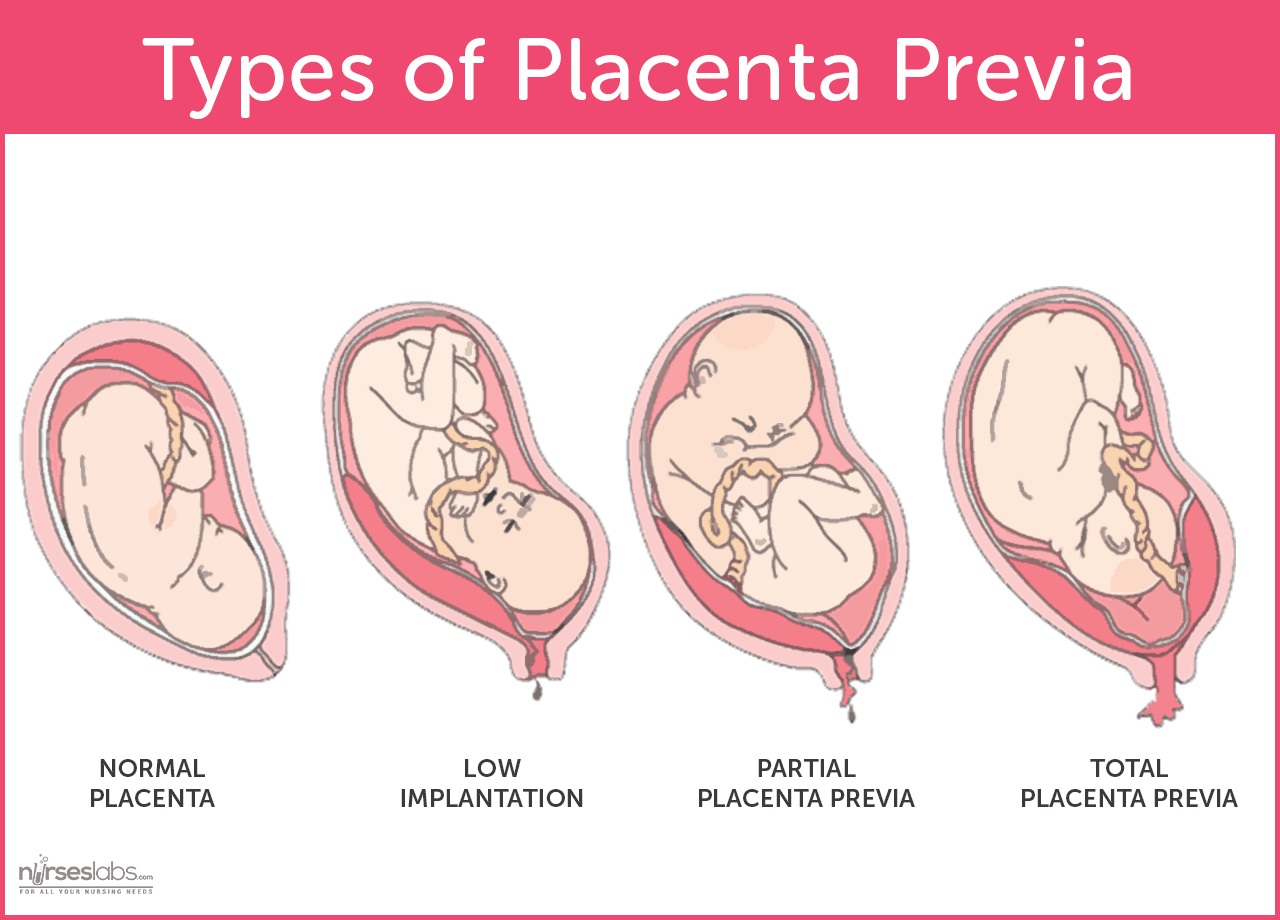 |
| Various
degrees of placenta previa. Photo by Nurseslabs |
Signs and Symptoms of Placenta Praevia
- Painless bleeding per vagina occurs at night.
- The uterus is not tender or tense on palpation.
- The fetal hand remains unengaged.
- There is malpresentation.
- The lie is oblique or transverse.
- The lie is unstable, usually in a multigravida.
Diagnosis
- Using ultrasonic scanning will confirm the existence of placenta praevia and establish its degree.
- The color of the blood is bright red, denoting fresh bleeding.
Assessment
If the haemorrhage is slight, the mothers blood pressure, respiratory rate and pulse rate may be normal.
In severe haemorrhage;
- There is low blood pressure and the pulse rate is raised.
- Respiration is rapid.
- The mother’s skin color will be pale and her skin will be cold and moist.
- Vaginal examination should not be attempted.
Assessing the Fetal Condition
The mother should be asked whether fetal activity has been normal. Excessive or cessation of fetal movement is another indication of severe fetal hypoxia.
Management of Placenta Praevia
The management of placenta praevia depends on;
- The condition of the mother and fetus.
- The amount of bleeding.
- The stage of pregnancy.
Conservative management; It is appropriate if bleeding is slight and both mother and fetus are well.
- The woman will be kept in hospital at rest until bleeding has stopped.
- A speculum examination will have ruled out incidental causes.
- Ultrasound scan are repeated at intervals in order to observe the position of the placenta in relation to the cervical os.
If bleeding should occur or when the fetus is mature, an examination per vagina will be carried out under general anesthetic at operation room. If the placenta is felt, caesarean section will be performed without delay.
The nurse/midwife should be aware that even if vaginal delivery is achieved, there remains a danger of postpartum haemorrhage because the placenta has been situated in the lower segment.
Active management; severe vaginal bleeding will necessitate immediate delivery by caesarean section. This should take place in a unit with facilities for special area of the new born especially if the baby will be preterm.
Complications
- Postpartum haemorrhage; Oxytocin should be given as the baby is delivered. Occasionally, uncontrolled haemorrhage may continue and a caesarean hysterectomy may be required.
- Maternal Shock
- Maternal death
- Fetal hypoxia due to placental separation
- Fetal death
PLACENTAL ABRUPTION
Placental abruption is premature separation of a normally situated placenta occurring after the 28th week of pregnancy. The etiology of this type of haemorrhage is not always clear but it is often associated with pregnancy induced hypertension or with a sudden reduction in uterine size. Rarely, direct trauma to the abdomen may partially dislodge the placenta.
Placenta abruption is an accidental occurrence of haemorrhage in about 2% of all pregnancies. Partial separation of the placenta causes bleeding from the maternal venous sinuses in the placental bed. Further bleeding continues to separate the placenta to a greater or lesser degree.
Types of Placental Abruption
The blood loss of the placenta abruption may be defined as revealed, concealed or mixed haemorrhage. An alternative classification based on the degree of separation and therefore related to the condition of mother and baby is; mild, moderate and severe haemorrhage.
Concealed Haemorrhage
- Blood is retained behind the placenta.
- The mother will have all the signs and symptoms of hypovolaemic shock.
- It causes uterine enlargement and extreme pain.
- The uterus appears bruised & oedematous.
Revealed Haemorrhage
Blood flows to the externally. There is no blood accumulated behind the placenta.
Mixed Haemorrhage
is a blend of the two situations above, some of the blood drains via the vagina and some is retained behind the placenta.
 | |
| Various degrees of placenta abruption. Photo by SEIF & ASSOCIATES |
Assessment of the Mother’s condition
There may be history of pregnancy induced hypertension, if there is placental separation after the birth of a first twin or loss of copious amounts of amniotic fluid during rupture of amniotic membrane.
If the blood is revealed;
More severe degrees are associated with abdominal pain, the uterus has a hard consistency and there is a guarding on palpation of the abdomen. Fetal parts may not be palpable and the fetal heart is unlikely to be heard with a fetal stethoscope.
Management
- Any woman with a history suggestive of placenta abruption needs to be attended to by a consultant obstetric unit.
- Pain exacerbates shock and should be alleviated.
- Secure intravenous infusion.
Observation
- Vital signs should be recorded.
- Urinary output should be accurately assessed.
- Fluid intake must also be recorded and balanced accurately.
- If the fetus is alive, the fetal heart rate should be monitored continuously.
- Any deterioration in the maternal or fetal condition must be immediately reported to the obstetrician.
Mothers who have passed the 37th week of pregnancy will have an amniotomy to induce labour. However, mothers who have not passed the 37th week may be cared for in an antenatal area for a few days and assessed for risks. Further bleeding or fetal distress may indicate that a caesarean section is necessary.
With moderate separation of the placenta, up to 1000mls of blood may be lost and in severe separation of the placenta, about 2000mls of blood or more is lost from the circulation.
Complications
- Coagulation defects
- Renal failure and pituitary failure
- Postpartum haemorrhage
Read Also
Pregnancy Induced Hypertension (PIH)Abortion
Ectopic Pregnancy
Postpartum Haemorrhage





0 Comments